Legionellosis is an infection caused by the bacterium Legionella. There are at least 46 species and 70 subgroups (serogroups). Approximately half of the species may cause human disease, but around 90% of all infections are caused by just one: Legionella pneumophila.
The bacterium was named Legionella pneumophila after a 1976 outbreak in Philadelphia during an American Legion convention. The outbreak, a mysterious calamity from an unknown cause which received wide coverage in the press, infected at least 239 people. It began when a number of attendees developed serious pneumonia. The pneumonia did not respond to conventional medical treatment, and 34 people died. Initially, it was not known whether the pneumonia was caused by infection or by chemical poisoning. After an extensive investigation, the illness was traced to previously unknown bacteria that were found growing in the HVAC system at one of the convention hotels.
Legionellosis is not spread by person-to-person contact. Legionellosis is caused by inhaling airborne droplets of water containing Legionella bacteria. The diagnosis of Legionellosis requires specialized tests not routinely performed on persons with pneumonia or fever.
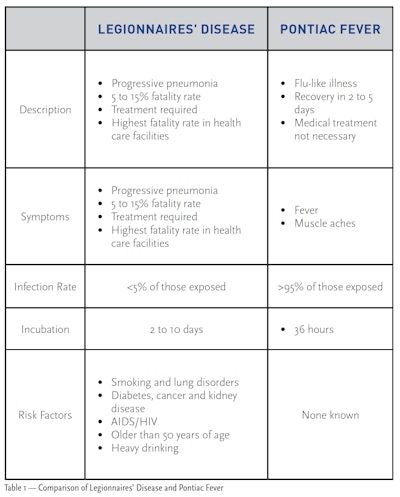
Legionellosis can occur in two forms. The most serious form is Legionnaires’ disease. Legionnaires’ disease is a severe form of pneumonia, and it can be fatal, especially to smokers and individuals with weakened immune systems. Individuals with higher risk factors require prompt medical treatment or the prognosis can be dire. The second form of Legionellosis is Pontiac fever, which is a mild infection and has symptoms similar to the flu. Individuals recover quickly from Pontiac fever and do not usually require medical treatment.
Where Does it Come From?
Current studies show that Legionella bacteria are widespread in nature; more than 40% of all freshwater bodies contain Legionella bacteria. The bacteria most likely enter man-made systems, such as HVAC systems, water heaters and spas, via the fill water. Legionella bacteria have a special lifestyle and unique nutritional requirements. Legionella bacteria grow only when other microorganisms are present. The other microorganisms supply nutrients for the Legionella. Most of the time, the Legionella bacteria live as parasites inside of protozoa, especially amoeba. Sometimes Legionella grow as small colonies inside biofilm with other bacteria and fungi. Periodically, some of the Legionella break out of the protozoa or the biofilm and randomly swim in the water. It is these free-swimming Legionella cells that can cause Legionellosis.
Legionella are found only in wet locations, and they die when their environment dries out. The Legionella bacteria grow slowly at temperatures under 61 degrees Fahrenheit, but thrive when the temperature is between 90 and 106 degrees Fahrenheit.
Legionellosis Cases
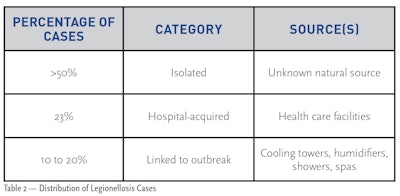
The U.S. Centers for Disease Control and Prevention (CDC) estimates that there are between 8,000 and 18,000 cases of Legionellosis in the U.S. every year. Public health officials estimate that less than 10% of all cases are reported. According to the CDC, the fatality rate is approximately 10% for individuals who contract Legionnaires’ disease. The majority of Legionellosis infections are caused by accidental contact with the bacteria in natural bodies of water such as lakes or rivers.
The second largest source of infection is health care facilities such as hospitals and nursing homes. The fatality rate for these infections can be as high as 50%. This is not surprising in that these individuals have underlying health issues, which frequently include weakened immune systems. Engineered water systems, such as cooling towers and humidifiers, are the major source of infections.
A small number of cases have been traced to showers and spas. In spas, Legionella become trapped in the bubbles from aeration. When the bubbles break the surface, they burst and release fine droplets that contain the bacteria. Spa users and others in the vicinity inhale the airborne droplets into their lungs, where the bacteria produce an infection. It is likely that the majority of infections from contaminated spas are Pontiac fever, the less severe form of Legionellosis. Legionella bacteria have not been found in spas that have a properly maintained disinfectant concentration. Swimming pools have not been linked with outbreaks.
Examples of Outbreaks from Spas and Portable Hot Tubs
The following well-publicized cases are typical Legionellosis outbreaks from spas. According to CDC Surveillance Summary data, outbreaks of this type continue to occur as a result of inadequate sanitation.
Case 1. In 1994, an outbreak occurred on a cruise ship sailing between New York City and Bermuda. A clinical investigation of the infected passengers confirmed 14 cases. One person died. The investigation showed that the ship’s spa was the source of the outbreak. The spa’s sand filter was infested with microorganisms, including Legionella pneumophila. The infestation developed because the sanitizer concentration had not been properly maintained.
Further investigation indicated that at least 28 passengers on nine previous cruises had also developed Legionellosis.
Note: After this outbreak, the CDC developed operational guidelines for spas on cruise ships. A link to the Vessel Sanitation Program operational manual is included in the references of this article.
Case 2. In 1996, an outbreak of 23 cases and two deaths was reported in Virginia. Twenty-two of the individuals required hospitalization. The mean age of the victims was 65. A clinical investigation traced the cases to a large home improvement center. DNA evidence positively traced the bacteria to a display spa in the store. The spa had been filled with drinking water but was never treated with a sanitizer. All patients reported being in the vicinity of the spa. The average time spent in the store was 79 minutes. Several patients spent 10 minutes in the spa display area. Four patients reported only walking by the spa display.
Case 3. In 1999, a total of 188 cases of Legionnaires’ disease and 15 deaths were reported in the Netherlands during an outbreak that occurred at a large flower and consumer show. Public health authorities began an extensive investigation after receiving reports of numerous cases of severe pneumonia. Although several possible water handling systems were involved, the evidence implicated a display spa. The spa was filled with water and held at 99 degrees Fahrenheit four days prior to the show. The spa was never treated with a sanitizer.
Case 4. In 2019, a total of 136 confirmed and 35 suspected cases of Legionellosis were reported after the North Carolina Mountain State Fair. This outbreak included 96 individuals that were hospitalized and 4 deaths. Because of the temporary nature of the fair, the investigation was not initiated before the fair had ended. The suspected source of the outbreak was display spas that had not been properly disinfected and maintained.
How Do You Control It?
Legionella bacteria are easily controlled if adequate sanitizer concentration is maintained at all times. No outbreaks have occurred when the water in the spa is properly maintained. Legionella and many other bacteria can quickly develop into very large colonies if the disinfectant/sanitizer level is not sufficient. This is especially true in spas with bathers. The organic load (body oils, perspiration, urine, feces and cosmetics) in these spas provides a high concentration of nutrients for microorganisms. The warm temperature, coupled with organic load, allows microorganisms to develop large colonies rapidly.
The U.S. Environmental Protection Agency (EPA) regulates products that control bacteria in swimming pools and spas. Those products registered by the EPA as disinfectants or sanitizers have been proven to adequately control bacteria in swimming pools and spas. A number of treatments are sold that claim to control bacteria but that have not been registered by the EPA, and the ability of these products to control bacteria has not been independently verified. Therefore, these products may not provide the necessary control of disease-causing bacteria. The PHTA recommends that all spa and portable hot tub operators:
- Use an EPA-registered disinfectant/ sanitizer. The product label will use one of these two words.
- Follow the label directions.
- Maintain the concentration of the disinfectant/sanitizer specified on the label at all times.
- Maintain the pH between 7.2 and 7.8.
- Perform regular oxidation and water replacement.
- Replace water frequently in heavily used spas and commercial spas.
- Drain, clean and refill lightly used residential spas every three months.
If an outbreak is confirmed or suspected, the spa must be closed and sanitized at once. Follow these steps below:
- Close the spa immediately.
- Turn off the blowers.
- If the spa is indoors, make certain that air for the spa room does not circulate into the rest of the facility through the HVAC system.
- Replace the filter cartridges or filter media.
- Chemically clean the filter housing and all accessible areas. Disinfecting bathroom cleaners are suitable for most spas. The area should be rinsed with tap water and the rinse water discarded before the spa is refilled.
- Sanitize the spa (see Decontamination of Spas and Wading (Kiddie) Pools Fact Sheet).
- Going forward, maintain the sanitizer level in the water at all times.
References
- Legionella information from the CDC
- CDC 1994. Update: Outbreaks of Legionnaires’ Disease Associated with a Cruise Ship, 1994. MMWR 43:574-575
- CDC 1996. Legionnaires’ Disease Associated with a Whirlpool Spa Display – Virginia, September-October, 1996. MMWR 46:83-86
- CDC 1997. Respiratory Infection – Pennsylvania. MMWR 46:49-56
- CDC 2000. Legionnaires’ Disease Associated With Potting Soil – California, Oregon, and Washington, May-June 2000. MMWR 49: 777- 778
- CDC 2018 Vessel Sanitation Program Operations Manual
- CDC 2001. Outbreak of Legionnaires’ Disease Among Automotive Plant Workers - Ohio, 2001. MMWR 50: 357-359
- Boer, Jeroen W. Den, et al, A Large Outbreak of Legionnaires’ Disease at a Flower Show, the Netherlands, 1999. Emerging Infectious Diseases 8: 37-43
- Fields, Barry. 1997. Legionellae and Legionnaires’ Disease, p.666-675. In C. J. Hurst, G. R. Knudson, M. J. McInerney, L. D. Stetzenbach, and M. V. Walter (ed.), Manual of Environmental Microbiology. American Society for Microbiology, Washington, D.C.
- CDC 2014. Recreational Water–Associated Disease Outbreaks — United States, 2009–2010, MMWR / January 10, 2014 / Vol. 63 / No. 1
- U.S. Environmental Protection Agency. Legionella: Human Health Criteria Document November 1999
- U.S. Environmental Protection Agency. March 2001. Legionella: Drinking Water Health Advisory
- World Health Organization. 2006. Guidelines for safe recreational water environments VOLUME 2 SWIMMING POOLS AND SIMILAR ENVIRONMENTS
- Violations Identified from Routine Swimming Pool Inspections --- Selected States and Counties, United States, 2008, MMWR May 21, 2010 / 59(19);582-587
- Legionnaires’ disease outbreak associated with the North Carolina Mountain State Fair, 2019, North Carolina Department of Health and Human Services January 30, 2020
- PHTA Fact Sheet. Decontamination of Spas and Wading (Kiddie) Pools Fact Sheet.
- Certified Pool & Spa Operator™(CPO) Handbook. Pool & Hot Tub Alliance, Alexandria, Va.
- ANSI/APSP/ICC-11 2019, American National Standard for Water Quality in Public Pools and Spas, Appendix A, Rationales for chemical operational procedures
This article first appeared in the October 2022 issue of AQUA Magazine — the top resource for retailers, builders and service pros in the pool and spa industry. Subscriptions to the print magazine are free to all industry professionals. Click here to subscribe.