Recreational Water Illnesses (RWIs) are a broad group of assorted infections and illnesses that result from exposure to pathogens or exposure to chemicals in aquatic venues intended for recreational use and entertainment. This article provides a general overview of only infectious RWIs associated with treated recreational water. RWIs do not include any illnesses from drinking water or water used in industrial processes (e.g., cooling and processing).
Recreational water itself is a broad category of venues that includes treated venues (e.g., swimming pools, spas, aquatic parks) as well as untreated natural waters (e.g., oceans, lakes, rivers, streams). Swimming is the fourth most popular recreational activity in the U.S. with over 301 million swims each year (U.S. Bureau of Census, 2012). Considering the popularity of swimming, the number of reported RWIs in treated venues (e.g., swimming pools, spas, aquatic parks) is quite low (Hlavsa, 2021).
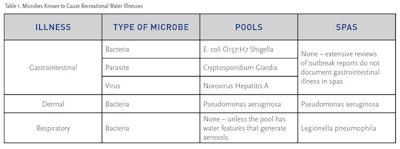
TYPES OF MICROBES THAT CAUSE RWIS
RWIs are caused by a small number of microbes of several different types (Table 1). All of the germs that cause RWIs are specialized in their ability to be transmitted in water. The gastrointestinal illness microbes are able to cause illness when as few as 10 cells or particles are swallowed. A typical mouthful of water swallowed by a swimmer is about 1 ounce (30 mL). If the concentration of one of these germs is 10 cells or particles for each 1 ounce of water, the water will still be clear. So even if the water is crystal clear, there is no guarantee that water does not contain one of these germs. The list of microbes in Table 1 accounts for at least 99% of the recognized RWIs.
All of the microbes that cause gastrointestinal illness cause considerable discomfort but rarely cause fatalities. E. coli O157:H7 infections in young children can cause kidney failure and lead to death if not promptly treated. All of these microbes can cause serious and persistent illness in immunocompromised individuals.
Pseudomonas aeruginosa (P. aeruginosa) is the only pathogen that causes dermal infections, which includes ear infections. It is also the only pathogen that causes illnesses in both swimming pools and spas. P. aeruginosa was first recognized as a dermal pathogen shortly after hot tubs became popular in the early 1980s. Other species of Pseudomonas do exist but are not known to cause RWIs. Since P. aeruginosa cases are not reportable to the U.S. Centers for Disease Control and Prevention (CDC) compared with other RWI microbes, the incidence is likely higher. Prior to the early 1980s, most of the literature considered Staphylococcus aureus (Staph) a cause of dermal infections from swimming pools. A complete review of the CDC’s RWI outbreaks since 1978 does not show a single report of Staph infections from pools or spas (RWI Manual).
Legionella pneumophila (L. pneumophila) is the only recognized pathogen that causes respiratory infections. To cause a respiratory infection, cells of L. pneumophila must be inhaled. The operating conditions of spas provide an ideal combination of conditions for growth for this germ, as L. pneumophila thrives in warm water. Legionella causes two forms of disease. Pontiac Fever is a mild illness while Legionnaires’ Disease is a severe pneumonia that can be fatal in up to 40% of cases. Because pools have cooler water and lack vigorous aerosolproducing features (e.g., misters and blowers), L. pneumophila RWI outbreaks do not occur in swimming pools.
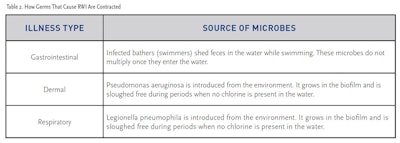
METHODS OF CONTRACTING RWIS
RWI infections begin when the concentration of the germ is above some specific concentration, referred to as the minimum infective dose, and the infective dose is introduced to the human by the correct route of exposure. For example, the infective dose of E. coli O157:H7 is about 10 cells; therefore, if 110 cells of E. coli O157:H7 are swallowed, there is a very high likelihood that the person will become ill. But if the same amount of E. coli O157:H7 contacts only the skin, the person will not become ill. This is because these microbes grow only in certain areas of the human body (RWI Manual).
HOW THE MICROBES THAT CAUSE RWIS ARE CONTROLLED
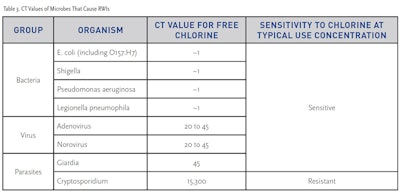
The primary means of controlling disease transmission in pools is free chlorine. Each type of microbe has a different physical structure that produces a unique level of resistance to the action of chlorine. This resistance to chlorine is measured by how long it takes a measured concentration of chlorine to kill, or deactivate, the cells in a measured number of minutes. The result is expressed as a “CT” value. The lower the CT value, the more easily the microbe is killed. Conversely, the higher the CT value, the more difficult it is to kill the microbe. For example, the CT value of Giardia (Table 3) is 45. This means that a specified number of Giardia cysts will be inactivated by 1 ppm of chlorine in 45 minutes. But any combination of free chlorine concentration (C) multiplied by time (T) that equals 45 will provide the same level of inactivation. For example, if the pool was operating at 3.0 ppm of free chlorine and some Giardia was carried in by an infected swimmer, those Giardia cysts would be inactivated in 15 minutes (CPO Manual).
As seen in Table 3, all the microbes that cause RWI except for one, Cryptosporidium, are killed or inactivated quickly by standard concentrations of free chlorine. Cryptosporidium is highly resistant to free chlorine due to the physical structure of its cellular design. With its unique resistance to chlorine, any attempt to control outbreaks by this microbe using chlorine alone is not possible.
HOW OUTBREAKS OF RWI OCCUR
The CDC has been publishing surveillance summaries of RWI outbreaks since 1978. An extensive review of those surveillance summaries does not reveal a single incident of an outbreak of the chlorine-sensitive microbes when the chlorine concentration was shown to be 1.0 ppm or greater (Hlavsa, 2021; older surveillance summaries beginning at 1978 are located at www.CDC.gov/healthyswimming). A very well-documented field evaluation of chlorine effectiveness calculated that if the free chlorine concentration was 1.0 ppm or greater, there was a 99% chance that RWI outbreaks would be prevented (Esterman, 1984). A review of aquatic venue inspections has shown that facilities are failing to maintain adequate chlorination levels between 10 and 14% of the time (Hlavsa, 2013). RWIs due to chlorinesensitive microbes would be prevented if the free chlorine level is maintained at 1.0 ppm or greater.
The exception to this is Cryptosporidium. Cryptosporidium is so resistant to chlorine that if the pool were operating at 10 ppm free chlorine and a Cryptosporidium fecal accident occurred, it would take at least 1,530 minutes, or 25.5 hours, to inactivate enough of the oocysts for the water to be considered safe for swimming. As a comparison, under the exact 10 ppm of free chlorine with a Giardia fecal accident, the water would be considered safe after just 4.5 minutes. Outbreaks of Cryptosporidium continue for several days after the initial fecal accident until the concentration of infective oocysts slowly declines. If infected swimmers continue to use the facility, the outbreak can last for several weeks or months. To limit outbreaks of Cryptosporidium, advanced treatment systems, such as Secondary Disinfection Systems using UV or ozone as specified in ANSI/APSP/ ICC-11 American National Standard for Water Quality in Public Pools and Spas (2019) and the Model Aquatic Health Code (MAHC, 2018), must be utilized.
TREATMENT METHODS TO PREVENT RWI OUTBREAKS
- Employ trained lead operators
- Have adequately trained staff available during all hours of operation
- Instruct and enable 2nd and/or 3rd shift personnel to close the venue without the need to consult with the primary operator if the free chlorine concentration is below the minimum or there is a vomit or fecal accident
- Maintain at least 1.0 ppm of free chlorine at all times
- Test the water at appropriate intervals to ensure that the free chlorine concentration never falls below 1.0 ppm free chlorine during periods of high bather use
- Close the facility and evacuate all swimmers from the water IMMEDIATELY if:
- The free chlorine drops below 1.0 ppm of free chlorine
- The circulation system is not functioning properly
- The chlorine feeder system is not functioning properly
- There is any vomit in the water
- There is a formed fecal accident
- There is a diarrheal accident
Do not reopen the facility until the situation is properly resolved.
- In “increased risk aquatic venues” utilize properly sized Secondary Disinfection Systems, as detailed in ANSI/APSP/ICC-11 (2019) and the MAHC (2018). An “increased risk aquatic venue” is an aquatic venue which has an increased risk of microbial contamination due to its primary users being children under the age of five and/or people more susceptible to infection, such as therapy patients with open wounds. Examples of increased risk aquatic venues include spray pads, wading pools, therapy pools, and other aquatic venues designed for children under the age of five (Refer to ANSI/APSP/ICC-11, 2019).
- Consider using properly sized Supplemental and Secondary Disinfection Systems in all public swimming venues as appropriate, following manufacturer’s use instructions.
Methods to treat outbreaks must be tailored to the type of microbe involved. Additional information on remedial treatments is available from PHTA at www.PHTA.org.
REFERENCES
1. U.S. Census Bureau. Statistical abstract of the United States: 2012. Arts, recreation, and travel: Participation in selected sports activities 2009
2. Hlavsa MC, Aluko SK, Miller AD, Person J, Gerdes ME, Lee S, Laco JP, Hannapel EJ, and Hill VR. Outbreaks Associated with Treated Recreational Water — United States, 2015–2019. MMWR Morb Mortal Wkly Rep 2021;70(20):733–738. DOI: https://www.cdc.gov/ mmwr/volumes/70/wr/mm7020a1.htm
3. Recreational Water Illness. 2018. The National Swimming Pool Foundation.
4. Pool and Spa Operator Handbook. 2021. Pool and Hot Tub Alliance (also called the CPO Manual)
5. Model Aquatic Health Code, 3rd ed, 2018. US Centers for Disease Control and Prevention. https://www.cdc.gov/mahc/editions/current. html
6. ANSI/APSP/ICC-11 2019 American National Standard for Water Quality in Public Pools and Spas Pool and Hot Tub Alliance, 2019. www. phta.org
7. Esterman et. al 1984. Determinants of the Microbiological Characteristics of South Australian Swimming Pools. AEM 47(2):325–328
8. CDC. Violations identified from routine swimming pool inspections — selected states and counties, United States, 2008. MMWR Morb Mortal Wkly Rep. 2010;59(19):582-7.
9. Hlavsa MC, Gerth TR, Collier SA, Dunbar ER, Rao G, Epperson G, Bramlett B, Ludwig DF, Gomez D, Stansbury MM, Miller F, Warren J, Nichol J, Bowman H, Huynh B, Loewe KM, Vincent B, Tarrier AL, Shay T, Wright R, Brown AC, Kunz JM, Fullerton KE, Cope JR, Beach MJ. Immediate closures and violations identified during routine inspections of public aquatic facilities — Network for Aquatic Facility Inspection Surveillance, five states, 2013. MMWR Surveill Summ. 2016;65(No. SS-5):1–26.
ADDITIONAL INFORMATION FROM PHTA
1. “Pseudomonas aeruginosa” Fact Sheet, Pool and Hot Tub Alliance, 2017.
2. “E. coli O157:H7” Fact Sheet, Pool and Hot Tub Alliance, 2017.
3. Legionellosis” Fact Sheet, Pool and Hot Tub Alliance, 2017.
4. “Secondary vs. Supplemental Disinfection Systems” Fact Sheet, Pool and Hot Tub Alliance, 2020.
The PHTA Recreational Water Quality Committee
Jody O’Grady, Taylor Technologies, Inc., Chair
Terry Arko, HASA, Inc.
Kevin Cox, NSF International
Dr. James Egan, LaMotte Company
Philip Escobedo, Fluidra
Rich Gallo, Pure Swim, Inc.
Kenneth Gregory, Pentair Water Quality Systems
Dr. Christopher M. Kareis, Axiall, A Westlake Company
Dr. Joseph Laurino, Periodic Products, PHTA Board of Directors Liaison
Touraj Rowhani, Sigura
Terry Snow, TLS Pool Service / Independent Pool and Spa Service Association (IPSSA) Representative
Dr. Roy Vore, Vore & Associates LLC
John Weber, BioLab, Inc.
Voting Alternates:
Jeff Gaulding, BioLab, Inc.
Ellen Meyer, Sigura
Consultants:
Jana Auringer, Pebble Technology International
Beth Hamil, MicroPlasma Ozone Technologies, Inc.
David Oxley, Pinellas Aquatic Consultation and Education
Dr. Stanley Pickens, Swim-Chem Consulting Services, LLC
This article first appeared in the June 2022 issue of AQUA Magazine — the top resource for retailers, builders and service pros in the pool and spa industry. Subscriptions to the print magazine are free to all industry professionals. Click here to subscribe.